Where are the Non-Communicable Diseases in Universal Health Care?
By Yibeltal Mekennon, Key Correspondent for the Irish Forum for Global Health
Speaking at the Global Health Exchange conference this week, Professor Michael O’Toole described the rising burden of non-communicable diseases (NCDs) linked with nutrition. NCDs have become the largest cause of global mortality and morbidity in the past decade. The UN Declaration on the Prevention and Control of NCDs and the subsequent WHO Implementation Plan aim to decrease mortality from NCDs by 25% by the year 2025 worldwide. There has been limited attention and funding for NCD control strategies by many governments and the global community. This is a hindrance to successful implementation of global strategies, and during a series of presentations at the conference some key issues were addressed.
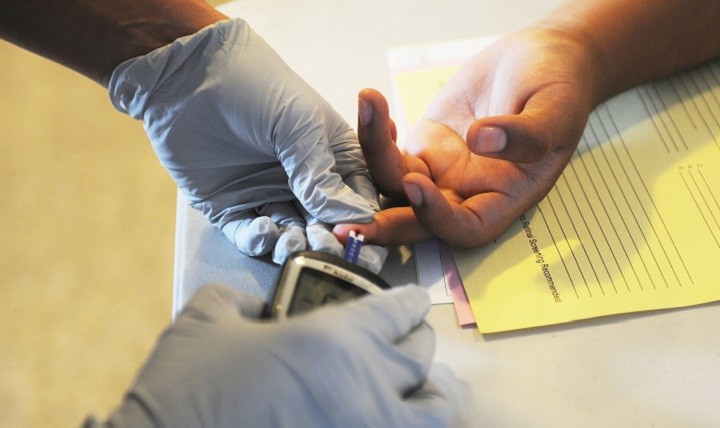
NCDs account for 70% of the 62 million annual global deaths. Low income countries contribute 80% to the overall burden. The major NCDs are cardiac disease, stroke, diabetes, respiratory disorders, and some cancers. Malnutrition is an important factor and interlinks with NCDs, where people born with low birth weight are at increased risk of metabolic syndrome and changing dietary habits, according to Professor Richard Firth, who spoke on The Global Diabetes Pandemic and West Africa. Tobacco, alcohol, diet and exercise are the four major risk factors that can be modified, “the best buys” and the most cost-efficient interventions in low-income countries.
Most sub-Saharan African (SSA) countries have seen an alarming rise in obesity and diabetes, indicative of a “global ‘diabesity’ pandemic” which, according to Professor Firth, is a prominent public health issue in West Africa – though holds true for a number of other SSA countries. He also describes consumption of meals with high sugar levels containing local carbohydrates as contributing to early development of these issues. The problem is exacerbated by SSA health systems often being ill-equipped to deal with the ever-increasing burden of these diseases. Many are in low-income regions, functioning in fragile states, or already overburdened with infectious disease and other emergencies.
Also, low awareness, lack of NCD literacy, and minimal early screening programs mean people seek care at advanced stages of already irreversible diseases. This results in increased care costs and reduced productivity. Professor Firth highlights that development aid has been prioritised for infectious diseases, namely HIV, TB, malaria and recently neglected tropical diseases. This leaves global and national level NCD strategies largely unfunded.
One case study shared during these sessions came from Togo. Here, there are promising results through concerted efforts in staff training, supply of simple diagnostic tools, appropriate medicines, and the education of patient communities about symptoms and early care-seeking. Patient outcomes have seen significant improvements.
According to Professor O’Toole:
“NCDs are here already, the global community has known that for some time… what we have found challenging is gearing our efforts and resources to tackle them at a global and local level.”
We should be able to draw from previous successful global engagements, such as the HIV pandemic, and progress on maternal and child health services. We must leave no one behind, including people suffering from or at risk of NCDs. The way forward has to include government strategies for better funding and integrating NCD comprehensive control and care to the primary level.
November 6th, 2018
Yibeltal Mekonnen is a medical doctor working at the Ethiopian Federal Ministry of Health. He has previously served as a general medical practitioner and lecturer in child health then as a medical director at a University Hospital. He is also affiliated to the Ethiopian Public Health association. He joined MSc in Global Health at Trinity College Dublin for the class of 2018/19. He has vast interest in global health issues including resilient health systems, organizational learning and universal health coverage. He has led a multi-disciplinary team in adapting a comprehensive primary health clinical guideline back in Ethiopia which currently under implementation. Yibeltal is an SOG Representative for Trinity, and is very excited to serve as a volunteer for the IFGH and eager to network with global health professionals.
CATEGORIES
- Restore Humanity Campaign
- Equity in Action Blog
- Training Programmes
- Sponsorship
- Vaccine Equity
- Get Global – Global Health Talks
- Student Outreach Team
- Get Global Young Professionals Talk Global Health
- Global Health Matters – Live Event Series
- Global Health Matters – IGHN Live Event Series
- An initiative of Irish Global Health Network
- ESTHER Ireland and ESTHER Alliance for Global Health Partnerships
- Global Health Matters – Webinar Series
- ESTHER
- IGHN Conferences
- Global Health Conference 2020
- Women in Global Health – Ireland Chapter
- ESTHER Partnerships
- Weekly Webinar Series
- 4th Global Forum on HRH
- Access to Medicines
- Archive Page Weekly COVID Webinars
- Clean Cooking 2019
- Climate Change and Health Conference 2017
- Conference Abstracts
- Conference Materials
- Covid FAQ
- COVID Funding Opportunities
- COVID-19
- COVID-19: Gender Resources
- Dashboard and online resources
- Education
- ESTHER Alliance
- Events
- Events & News
- Funding covid
- Global Health Exchange 2018
- Global Health Exchange 2019
- Global Health symposium 2019
- Health Workforce/HRH
- Homepage Featured
- Homepage recent posts
- IFGH 2011-2012 Conference and Events
- IFGH 2014 Conference
- IFGH Multimedia
- Irish AIDS Day 2017
- Irish News and Feeds
- Key Correspondent Articles
- Key Correspondent News
- Maternal Health
- Multimedia
- News
- News & Events
- Newsletter
- Opportunity
- Our LMIC's Resources for COVID19
- Partner Country News and Feeds
- Past Events
- Policy
- Presentations
- Recurring events
- Reports & Publications
- Research
- Resources
- Student Outreach Group
- Students Corner
- TEDTalks
- TRAINING COURSES FOR HEALTH CARE PROFESSIONALS
- Uncategorized
- Upcoming Events
RECENT POSTS

Impact testimonies- Lombani

Impact Testimony – Shadrick

Power, Inequality, Decolonisation – and Living My Recovery By Bronwyn April

Global Health Without Borders: Reflections on the Power of Diverse Voices

IGHNxEU – Empowering Women for a Healthier Europe

