Webinar 17: Men and COVID-19: How are men affected by COVID-19 and the response can better include them?
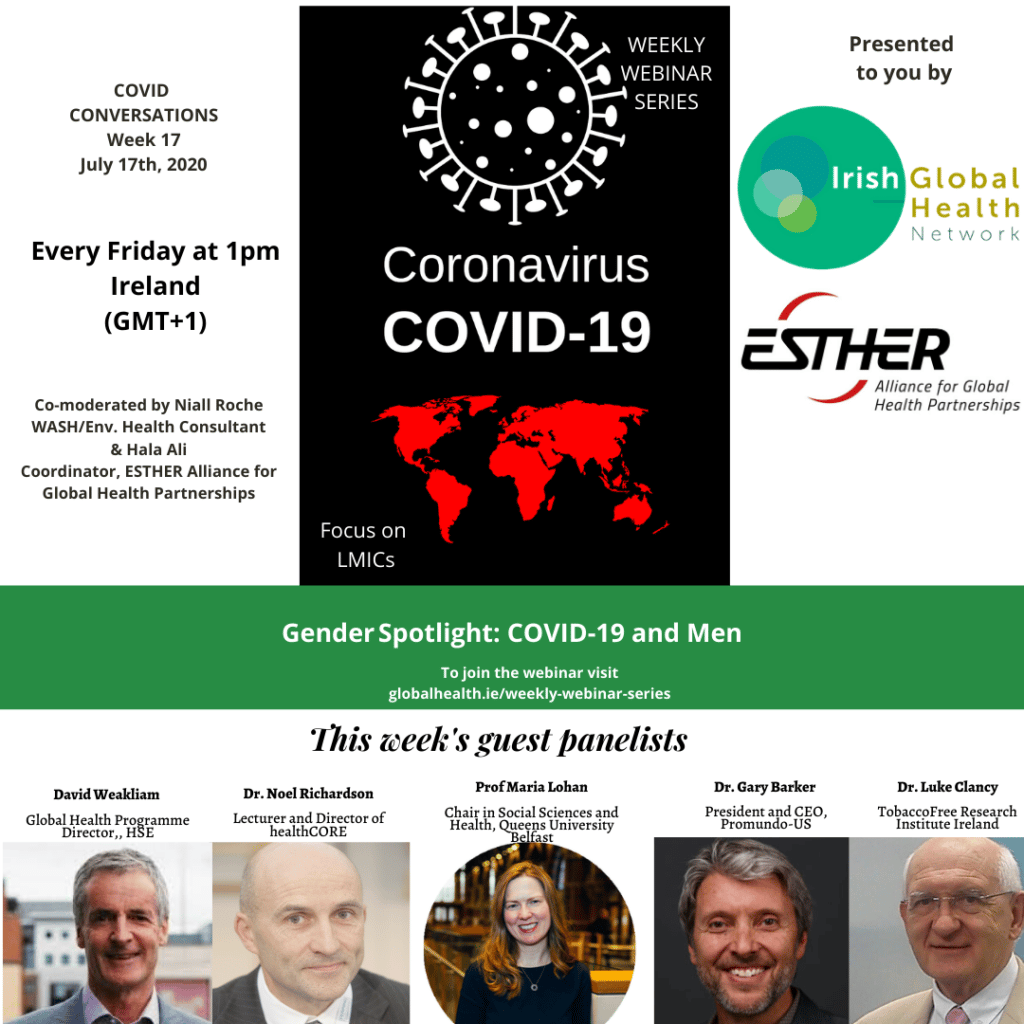 WEBINAR SERIES: WEEK SEVENTEEN Men and COVID-19: How are men affected by COVID-19 and the response can better include them?
WEBINAR SERIES: WEEK SEVENTEEN Men and COVID-19: How are men affected by COVID-19 and the response can better include them?
The full suite of resources shared by speakers is available under each of their individual recordings, along with a summary of the points they made. A full list of additional resources shared by participants and hosts during the webinar can be found at the bottom of the page.
VIEW THE WEBINARYour feedback is important to us so that we can continue to share learnings, insights and practices relevant to those working in the LMIC community. Please take the time to complete our evaluation at the button below so that we can continue to improve the series.
COMPLETE WEBINAR EVALUATIONINTRODUCTION:
Gender equality is a central component of any humanitarian to development response. In the context of COVID-19 this is also the case. Women and men, boys and girls are all affected by COVID-19. Much of the commentary so far indicates that women are more affected by COVID-19 in terms of high numbers of cases and serious secondary consequences around domestic violence for example. However, men seem more prone to severe episodes of the disease (perhaps related to diet and smoking) and more likely to die than women. Men also work in sectors of the economy, transport and construction for example, that might put them at a high risk.
This discussion put a specific focus on men, the impact of COVID-19 on them directly and indirectly. It explored how well the response is addressing the particular needs of men.
Our speakers were invited to address the following key questions: What disaggregated data exists on COVID-19 with respect to men? How is COVID-19 impacting on men and how are they coping? What should the response be doing more of to better meet the needs of men, women, boys and girls?
A SUMMARY OF POINTS MADE
Noel Richardson from IT Carlow who is Director of the National Centre for Men’s Health in Ireland. Dr. Noel Richardson has extensive experience in the area of men’s health at a research, policy and advocacy level. He was principal author of Ireland’s National Men’s Health Policy (2009) and co-author of the first European Union Report on Men’s Health (2011). He also collaborated on the WHO European Region Men’s Health Report and Men’s Health Strategy (2018).
Dr. Richardson opened with a call to focus on COVID-19 sex and gender differences in order to better guide both public health policy and responses, and to better understand the populations of men most impacted by the virus. He notes that Ireland was the first country to establish a National Men’s Health Policy and therefore this discussion is especially pertinent in the Irish context.
- It is important to remember not to fall into the trap of “competing victims rhetoric” when discussing gender issues. Instead, the aim should be to take into account sex and gender when responding to COVID-19
- First must differentiate sex and gender differences. Sex differences include biological, immunological and hormonal factors. Gender differences include lifestyle and health behaviour factors that are influenced by cultural norms
- COVID-19 prevention behaviours: with regards to handwashing and wearing masks, lower rates for men have been seen in some studies
- Intersectionality between gender and other social determinants of health that lead to additional risk — these factors exacerbated during the pandemic
- “A pandemic might potentially be a catalyst for positive change in men’s lives and present opportunities for reconfiguration of men’s roles”, for example balanced lives, divergence from the provider paradigm, assuming domestic and caregiver positions, enhanced community spirit
Professor Maria Lohan, Professor Maria Lohan is Chair in Social Sciences and Health, School of Nursing & Midwifery and Theme Lead for Maternal and Child Health at Queen’s University Belfast. Professor Lohan’s research team is dedicated to better understanding inequalities in health in society, especially in relation to improving men’s sexual health and involvement in reproduction and parenting.
Professor Maria Lohan began by providing context for her discussion, remarking that the UK government requested insight into the lower levels of adherence to public health guidelines displayed by men.
- Her team first sought out to confirm the problem through reviewing literature and discovered heterogeneous findings: some gender differences in social distancing, and reasonably strong evidence for men and low adherence to both hand-washing and isolation
- The focus then shifted to behaviour change, and a workshop with experts on men’s health was held. Generalisable strategies that were developed:
- “Show men positively doing the right thing in the company of other men and others”
- “Make adherence visible” in terms of media messaging through a photograph of men adhering
- “Make adherence desirable”
- “Use the science”
- Infrastructure is an important enabler, for example, mandatory face masks leads to higher adherence for men. Professor Lohan highlights the next step being legislation, especially to protect high-risk occupations
Gary Barker, President and CEO of Promundo-US. Promundo is an NGO which started in Brazil that now has 5 offices, and works internationally to engage men and boys in gender equality and carry out research on masculinities. He is co-founder of MenCare, a global campaign to promote men’s involvement as equitable caregivers. He leads the International Men and Gender Equality Survey, a study of men’s attitudes and behaviors related to violence, health, and fatherhood, carried out in nearly 50 countries.
Dr. Gary Barker started by acknowledging Promundo’s work in approaches to engage men in various areas such as violence prevention, care work, HIV, and sexual/reproductive health. Efforts have demonstrated limited success when utilising single messaging approaches instead of relational models which incorporate other influential individuals.
- The ‘Fatherhood and Couple Training Model’ in Rwanda aims to aid in couple communication as well as maternal, child and men’s health information delivery. This program evaluated by a randomised controlled trial design notably found a 40% decrease in partner violence. Overall, it was observed that “men’s behaviours changed to the degree that they felt responsible for and connected to others” and that a “collective sense of care” was necessary to overcome negative peer influence
- In Brazil, Dr. Barker worked in tandem with the healthcare system to develop an opt-out ‘Prenatal Health Protocol for Engaging Men’ as this is the principal primary care setting to find men attending. Men are encouraged to attend the prenatal visit, leading to a general health exam. This program seeks to alter the idea that men are at fault for not choosing to engage, and instead focus on transforming the health care system to better facilitate engagement
- ‘The Man Box Survey’ found associations between destructive behaviours and valuing harmful masculinity norms. Dr. Barker notes how men also form an identity around masculine norms and something must be offered in its place in order to shift away from these values
- ‘The MenCare Campaign’ is compiling tales of “men doing the right thing” in the context of caregiving
Professor Luke Clancy – Director General, TobaccoFree Research Institute Ireland (TFRI) Dublin and Consultant Respiratory Physician. Professor Luke Clancy is an academic physician with an international track record in the area of smoking and health and on the causes, management and prevention of respiratory diseases particularly air pollution, asthma, cancer and tuberculosis. He has considerable experience over the last 25 years in directing and coordinating research projects on these conditions.
Professor Luke Clancy opened with a stark contrast between the efforts directed towards COVID-19 and the lack of efforts targeting smoking, despite the substantially higher mortality rate of smoking and preventability of smoking.
- The tobacco crisis has many complexities, including the tobacco industry seeking to profit from addiction. To capitalise off of early reports that noted fewer individuals with the virus were smokers, questions regarding protective effects were raised. However, other associations such as healthcare worker being less likely to smoke influence the results
- Despite the uncertainty revolving around these claims, Professor Clancy urges to remember that there are certainties including: smoking being bad for your health and smoking as a causative factor for co-morbidities associated with mortality
- Data regarding prevalence of smoking and COVID is not clear, yet severity of COVID-19 is clearly related to smoking
- Professor Clancy expresses that he believed the pandemic “…was a huge opportunity for smoking cessation [and he] can’t understand how there hasn’t been more emphasis on it”. He further questions why smoking cessation did not transition to being offered online throughout lockdown
Webinar Anchor: David Weakliam, Global Health Lead, HSE
To view his contribution, click here
Download David’s Presentation HERE
- The COVID-19 pandemic is ongoing and deaths are increasing
- Africa Center for Strategic Studies Report – ‘Africa’s Varied COVID Landscapes’: Unable to generalise case findings due to diversity in the countries, therefore “Seven COVID-19 Profiles” were developed in hopes to identify patterns and to possibly guide future predictions
- Gender and COVID-19: Susceptibility and vulnerability to the virus are sex and gender dependent. Further, the social and economic impact is experienced differently by men and women. Greater attention has been focused on the impact of COVID-19 on women
- Global Health 5050 — COVID-19 sex-disaggregated data: Global ‘deaths among confirmed cases Male-Female ratio’ shows that men are more likely to die than women from COVID-19 if contracted. The important gender factors are: “risk of exposure, response to disease, pathways of care, gender of HCWs”
Further Resources:
- Gender-Transformative Bandebereho Couples’ Intervention to Promote Male Engagement in Reproductive and Maternal Health and Violence Prevention in Rwanda: Findings From a Randomized Controlled Trial
- ‘Beyond the prostate: Brazil’s national healthcare policy for men (PNAISH)’, EMERGE Case Study 1
- The Cost of the Man Box: A study on the economic impacts of harmful masculine stereotypes in the United States
- Caring Under COVID-19: How the Pandemic Is – and Is Not – Changing Unpaid Care and Domestic Work Responsibilities in the United States
- Noel Richardson discusses the state of Irish men’s health
- WHO Gender and COVID-19
COVID-19 sex-disaggregated data tracker
- Summary report on considering gender in COVID-19 hygiene promotion programmes
- YOUNG MEN AND UNINTENDED PREGNANCY – IF I WERE JACK
CATEGORIES
- Restore Humanity Campaign
- Equity in Action Blog
- Training Programmes
- Sponsorship
- Vaccine Equity
- Get Global – Global Health Talks
- Student Outreach Team
- Get Global Young Professionals Talk Global Health
- Global Health Matters – Live Event Series
- Global Health Matters – IGHN Live Event Series
- An initiative of Irish Global Health Network
- ESTHER Ireland and ESTHER Alliance for Global Health Partnerships
- Global Health Matters – Webinar Series
- ESTHER
- IGHN Conferences
- Global Health Conference 2020
- Women in Global Health – Ireland Chapter
- ESTHER Partnerships
- Weekly Webinar Series
- 4th Global Forum on HRH
- Access to Medicines
- Archive Page Weekly COVID Webinars
- Clean Cooking 2019
- Climate Change and Health Conference 2017
- Conference Abstracts
- Conference Materials
- Covid FAQ
- COVID Funding Opportunities
- COVID-19
- COVID-19: Gender Resources
- Dashboard and online resources
- Education
- ESTHER Alliance
- Events
- Events & News
- Funding covid
- Global Health Exchange 2018
- Global Health Exchange 2019
- Global Health symposium 2019
- Health Workforce/HRH
- Homepage Featured
- Homepage recent posts
- IFGH 2011-2012 Conference and Events
- IFGH 2014 Conference
- IFGH Multimedia
- Irish AIDS Day 2017
- Irish News and Feeds
- Key Correspondent Articles
- Key Correspondent News
- Maternal Health
- Multimedia
- News
- News & Events
- Newsletter
- Opportunity
- Our LMIC's Resources for COVID19
- Partner Country News and Feeds
- Past Events
- Policy
- Presentations
- Recurring events
- Reports & Publications
- Research
- Resources
- Student Outreach Group
- Students Corner
- TEDTalks
- TRAINING COURSES FOR HEALTH CARE PROFESSIONALS
- Uncategorized
- Upcoming Events
RECENT POSTS

Impact testimonies- Lombani

Impact Testimony – Shadrick

Power, Inequality, Decolonisation – and Living My Recovery By Bronwyn April

Global Health Without Borders: Reflections on the Power of Diverse Voices

IGHNxEU – Empowering Women for a Healthier Europe

