Conversations on COVID-19 11th Webinar: The Broader Health & Health Systems Impacts of COVID-19 in LMICs
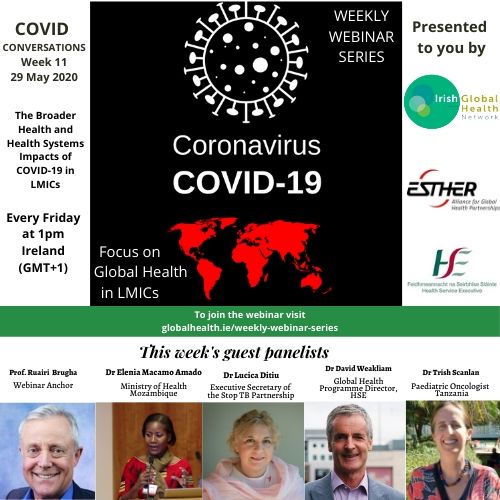 WEBINAR SERIES: WEEK ELEVEN The Broader Health & Health Systems Impacts of COVID-19 in Low- & Middle-Income Countries
WEBINAR SERIES: WEEK ELEVEN The Broader Health & Health Systems Impacts of COVID-19 in Low- & Middle-Income Countries
This week’s webinar was co-hosted by the Society of Occupational Medicine (SOM).
The eleventh webinar was held on Friday 29/05/2020 at 12:00 pm GMT/1PM Irish Time.
The full suite of resources shared by speakers is available under each of their individual recordings, along with a summary of the points they made. A full list of additional resources shared by participants and hosts during the webinar can be found at the bottom of the page.
VIEW THE WEBINARYour feedback is important to us so that we can continue to share learnings, insights and practices relevant to those working in the LMIC community. Please take the time to complete our evaluation at the button below so that we can continue to improve the series.
COMPLETE WEBINAR EVALUATIONA SUMMARY OF POINTS MADE
Dr. Elenia Macamo Amado, Ministry of Health, Mozambique
To view her contribution, click here
In Mozambique, there is a high prevalence of both TB and HIV in the general population, and malaria is a consistent concern. There also remains the drive to reduce rates of maternal/infant mortality. Therefore, hospitals did not close off to those presenting with these diseases, but efforts were taken early to ensure that COVID-19 patients were kept separate. People have been wary of coming to hospital for treatments in the atmosphere of COVID-19, and so accurate data has been difficult to track.
Advocacy and community collaboration is key to reduce disease burden. Mozambique is sharing protocols and collaborating with Portugal and with the WHO. Good planning/preparation along with the ability to adapt delivery of services during COVID-19 will be vital.
Dr. David Weakliam, Global Health Programme Director, HSE
To view his contribution, click here
Indirect effects of COVID-19 are becoming more apparent in both Ireland and in LMICs. Ireland recorded its first COVID-19 case on the 1st of March. Within 10 days, there were thousands of deaths throughout Europe. The strong Irish response is commendable, however it has also led to knock-on effects for health services. Non-essential services were delayed/suspended, but essential services were often also affected due to patient concerns about COVID-19 infection: 30% fewer emergency room admissions, fewer attending for cancer treatments etc.
Indirect effects of COVID-19 have even more impact in LMICs. COVID-19 has caused immunization services against other diseases to be disrupted in 68 countries worldwide. Disruption to TB treatment services will have huge effects of disease and mortality rates. True infection rates in Africa have been far less than those originally modeled (62 deaths reported on the 4th of June). Addressing the secondary effects of COVID-19 therefore must be made a priority. A health systems approach that focuses on protecting health workforce and on availability of medicines and equipment will be important in the near future.
These challenged can be viewed as an opportunity to provide healthcare in a better way; to act as a catalyst for more equitable service provision and to engage communities in the health system. Institutional partnerships provide huge opportunities to assist LMICs in achieving these developments too.
If you would like to know more about David Weakliam:
Dr. Lucica Ditiu, Executive Secretary of the Stop TB Partnership
To view her contribution, click here
As China is in the top 5 countries with the highest TB prevelance in the world, Stop TB Partnership were working closely with organisations in the country in early 2020. India has the highest TB disease burden, and is the only country with live TB diagnosis and demographic updates. There can be observed a 70% drop in TB diagnosis in India, and this can be extrapolated out globally.
Data on the effects of COVID-19 infection on those already affected by TB is still scarce. While initial data indicates that co-infection makes prognosis worse, secondary affects of COVID-19 can be far more detrimental. Many doctors who previously had been dealing with TB has been diverted to COVID-19 response. Increase in coronavirus cases and overcrowding can have an effect on infection control capabilities for other diseases, and for each month of lock-down implemented there is an impact for those suffering with other infectious diseases. Stop TB is conducting modelling studies for TB rates in several high-burden countries ie. Bangladesh, Kenya etc.
The combination of lack of PPE in health-care settings and fear of the disease among the general public has led to an increase of cases globally. Diagnosis & treatment of TB must continue throughout the pandemic, and some countries/areas have adapted to at-home treatments for 3 months. Measures taken to combat TB can and does inform the COVID-19 response, and COVID-19 has brought the attention of governments and the general public to the importance of health response and infection control.
For more information on STOB TB, CLICK HERE
Dr. Trish Scanlan, Paediatric oncologist, Muhimbili Hospital, Tanzania; Their Lives Matter (TLM), Tanzania
To view her contribution, click here
In Muhimbili National Hospital (largest government hospital in Tanzania), TLM provides cancer treatment free of charge to children. Outreach centres have also been developed across the country that are assisted in cancer treatments by TLM. The Muhimbili National Hospital-University of Medicine and Allied Health is partnered with Dar es Salaam & Our Lady’s Children’s Hospital, Crumlin, and is an accredited ESTHER Ireland partnership.
Trish’s hospital has followed much of Ireland’s response, reacting early to ensure protection of healthcare staff and vulnerable patients before cases were seen in the community. Ward spaces have been modified; fewer visitors are permitted; importance of mask-wearing and hand-hygiene practices has been re-emphasized; and there has been mobilization of the community to make masks and gowns.
Staff health and wellbeing, both mental and physical, is a top priority; arranging alternatives to public transport, facilitating small numbers, providing simple meals etc. creates good will and trust. Numbers of patients admitted has decreased due to COVID-19, and a decision was made not to test patients unless absolutely necessary. Many young patients live on these wards full-time for months; instead, the approach is to act as if every child and adult as COVID-19 positive. Early action has made a real difference; no staff have been very unwell on the ward, and fears have reduced.
- To find out more about Their Lives Matter, CLICK HERE
- Irish Times article featuring Trish Scanlon
Prof. Ruairi Brugha, Professor, Royal College of Surgeons in Ireland, Webinar Anchor
To view his contribution, click here
Download Ruairi’s Powerpoint Presentation
Ruairi’s Resources:
- HSE Resource
- COVID-19 Worldometer
- The potential effects of widespread community transmission of SARSCoV-2 infection in the WHO African Region: a predictive model
- Early estimates of the indirect effects of the coronavirus pandemic on maternal and child mortality in low- and middle-income countries
Further Resources:
- The relatively young and rural population may limit the spread and severity of COVID-19 in Africa: a modelling study
- New WHO estimates: Up to 190 000 people could die of COVID-19 in Africa if not controlled
- The Lancet – Has COVID-19 subverted global health?
COVID-19: Operational guidance for maintaining essential health services during an outbreak
- COVID-19: mortality, future years lost, and demographic structure. UN May 2020
- Report 19 – The Potential Impact of the COVID-19 Epidemic on HIV, TB and Malaria in Low- and Middle-Income Countries
- The Potential Impact of the COVID-19 Response on Tuberculosis in High-burden Countries: A Modelling Analysis
- Report 18 – The potential public health impact of COVID-19 on malaria in Africa
- Policy Brief: COVID-19 and the Need for Action on Mental Health
- Missionary Responses to Ebola Virus Crises
Resource suggested by Breda Gahan, Registered Nurse & Midwife:
CATEGORIES
- Restore Humanity Campaign
- Equity in Action Blog
- Training Programmes
- Sponsorship
- Vaccine Equity
- Get Global – Global Health Talks
- Student Outreach Team
- Get Global Young Professionals Talk Global Health
- Global Health Matters – Live Event Series
- Global Health Matters – IGHN Live Event Series
- An initiative of Irish Global Health Network
- ESTHER Ireland and ESTHER Alliance for Global Health Partnerships
- Global Health Matters – Webinar Series
- ESTHER
- IGHN Conferences
- Global Health Conference 2020
- Women in Global Health – Ireland Chapter
- ESTHER Partnerships
- Weekly Webinar Series
- 4th Global Forum on HRH
- Access to Medicines
- Archive Page Weekly COVID Webinars
- Clean Cooking 2019
- Climate Change and Health Conference 2017
- Conference Abstracts
- Conference Materials
- Covid FAQ
- COVID Funding Opportunities
- COVID-19
- COVID-19: Gender Resources
- Dashboard and online resources
- Education
- ESTHER Alliance
- Events
- Events & News
- Funding covid
- Global Health Exchange 2018
- Global Health Exchange 2019
- Global Health symposium 2019
- Health Workforce/HRH
- Homepage Featured
- Homepage recent posts
- IFGH 2011-2012 Conference and Events
- IFGH 2014 Conference
- IFGH Multimedia
- Irish AIDS Day 2017
- Irish News and Feeds
- Key Correspondent Articles
- Key Correspondent News
- Maternal Health
- Multimedia
- News
- News & Events
- Newsletter
- Opportunity
- Our LMIC's Resources for COVID19
- Partner Country News and Feeds
- Past Events
- Policy
- Presentations
- Recurring events
- Reports & Publications
- Research
- Resources
- Student Outreach Group
- Students Corner
- TEDTalks
- TRAINING COURSES FOR HEALTH CARE PROFESSIONALS
- Uncategorized
- Upcoming Events
RECENT POSTS

Impact testimonies- Lombani

Impact Testimony – Shadrick

Power, Inequality, Decolonisation – and Living My Recovery By Bronwyn April

Global Health Without Borders: Reflections on the Power of Diverse Voices

IGHNxEU – Empowering Women for a Healthier Europe

